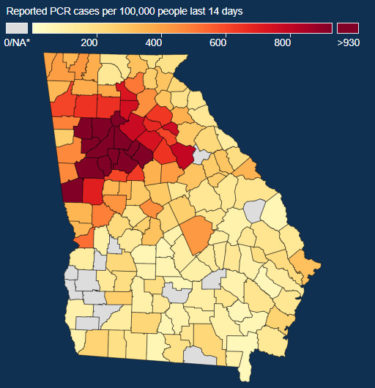
Close to 20,000 new Covid cases (including positives from antigen tests) were reported in Georgia on the last Wednesday of 2021, as new daily state records were being set. On the state virus map, metro Atlanta was covered by a deep, dangerous red color, signifying high rates of infection.
People were scrambling to get Covid tests, and many were forced to reconsider their New Year’s plans. Six hospital systems in the metro Atlanta area jointly announced Wednesday that had experienced 100 to 200 percent increases in Covid hospitalizations in the past eight days, with the vast majority of inpatients being unvaccinated.
Almost two years into the pandemic, Covid continued to dominate headlines . . . and it dominates our list of the Top 10 Georgia health care stories of 2021.
Vaccines became a key weapon. Matching the startling speed of Covid vaccine development, drug process development services companies produced and shipped millions of doses to the nation in 2021. Georgians from the outset began getting in line for shots, and research showed that vaccinated people had a much better chance of escaping hospitalization and death. Yet at the end of the year, just barely over 50 percent of Georgians were fully vaccinated, even as booster shots were being given to increase immunity.
The virus adapted. After the first months of the pandemic, variants of Covid began to emerge, highlighting the disease’s complexity. Georgia suffered through a deadly surge driven by the Delta variant. As that subsided, a new variant, Omicron, emerged toward the end of the year. Omicron helped fuel a daily record of Covid cases being reported, both in the U.S. and in Georgia. Hospitals again were seeing their number of virus patients increase.
Covid created more health worker shortages. Nursing staffs in hospitals shrank as RNs left for less perilous work environments and even retired. Hospitals began offering unprecedented bonuses to attract nurses. Covid also forced shortages of caregivers for people with disabilities getting home care. And state-run psychiatric hospitals faced alarming shortages of employees.
Kemp waivers ran into trouble. After the Biden administration took office, the federal Centers for Medicare and Medicaid Services began questioning the work requirements in Gov. Brian Kemp’s proposal for increasing Medicaid enrollment in Georgia. Then, shortly before Christmas, the agency rejected those eligibility restrictions. Meanwhile, CMS also asked tough questions about the GOP governor’s other waiver request, to replace healthcare.gov with an insurance portal privately run by insurers and brokers.

ACA marketplace enrollment soared. Federal health officials announced record enrollment in government-affiliated marketplaces that let people buy health coverage. That high mark that was partly fueled by jumps in sign-ups in Georgia and the 11 other states that had not expanded Medicaid under the Affordable Care Act. Georgia reported a record 653,000 enrollees, as the number of insurance options increased, buttressed by more help from ACA counselors (“navigators”) and enhanced discounts for some marketplace customers.
Abrams entered gubernatorial race. Democrat Stacey Abrams, who narrowly lost to Republican Brian Kemp in 2018, announced she was running for governor again in 2022. With Abrams’ advocacy of Medicaid expansion and other policies that Gov. Kemp and his GOP allies have rejected, this signaled that health care could be a pivotal issue in the contest.
Expired contracts and frustrated customers. More contracts between giant insurers and hospital systems nationally were being severed without a renewal agreement, and those disruptions played out in Georgia as well. Wellstar’s contract with UnitedHealthcare ended in October, and Anthem Blue Cross Blue Shield was heading for a Jan. 1 breakup with Northside Hospital.

Rural health problems persisted. Extra Covid funding helped stave off closures of rural hospitals across the nation, but there were many pockets in Georgia where medical services remained scarce. Some communities began looking to establish stand-alone rural emergency hospitals to fill the holes left by shuttered hospitals.

Hospital consolidation resumed. Piedmont Healthcare added four Georgia hospitals, buying them from HCA. Piedmont also began closing in on University Hospital in Augusta. Meanwhile, in Rome, Atrium Health took over Floyd Medical Center, while AdventHealth acquired Redmond Regional Medical Center. Such moves added bargaining clout to hospital systems seeking higher reimbursements from health insurers.

EPA widened probe of lead in Atlanta soil. The federal EPA expanded its investigation of a large swath of the low-income English Avenue neighborhood for lead in the soil. Meanwhile, a Georgia House study committee produced a series of recommendations to beef up state law aimed at protecting people from lead poisoning.
Monkeypox scare hit Georgia. Public Health officials reported that 43 people in Georgia were monitored in July for monkeypox. They had been exposed to an air traveler infected with the rare disease while the person was flying from Nigeria to Atlanta and then to Dallas. None of the Georgians turned out to be infected. Monkeypox originates in various wild animals, not only monkeys, and can be transmitted if a person comes into contact with the virus from an infected animal, an infected person or contaminated materials.

