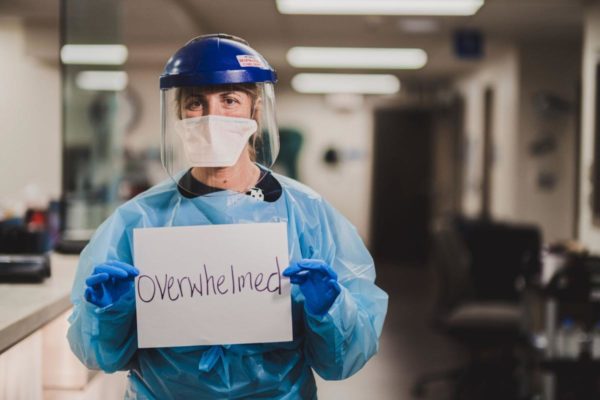
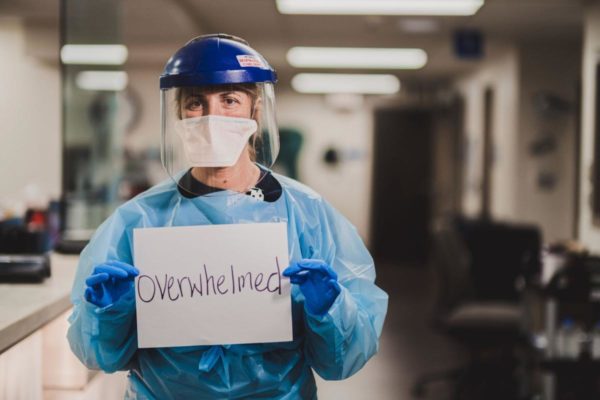
The impact of COVID-19 overwhelmed the news cycle – and public discussion — during 2020.
That’s why it’s difficult to include any other topics in our annual Top 10 Georgia health care stories of the year.
Nevertheless, we put COVID-related stories in our first five slots. It very well could have been all 10.
Here’s our list. Let us know what you think – and what we missed.
(No. 1) Albany became an early hot spot for the virus. Phoebe Putney Memorial Hospital in Albany was flooded with coronavirus patients in March after the disease spread among mourners at two crowded funerals in the southwest Georgia city. The uncontrolled spread of the disease in the community gave Albany and Dougherty County one of the highest per-capita infection rates in the entire nation in the pandemic’s early stages. Phoebe’s CEO said the surge rapidly consumed hospital supplies of personal protective equipment: “We went through six months’ worth in five days,’’ Scott Steiner told GHN.
2. December brought record cases and hospitalizations just as vaccines finally began to arrive. Hospital ICUs filled up as Georgia reported single-day records for new COVID cases, including more than 10,600 on Christmas Eve. COVID hospitalizations in the holiday season surpassed records set during the summer. As these numbers grew more alarming, experts hoped for a better 2021 as the first shots of COVID vaccine were given to medical workers.
3. The disease hit disproportionately hard in African-American and Latino communities, and in rural areas. Communities of color in Georgia and the U.S. drew higher percentages of COVID cases and deaths. One possible reason was that more people of color were serving as essential workers, directly in the path of the virus, USA Today reported. Decades of discrimination in housing has put people of color into dense neighborhoods, fueling the spread of the virus. Older people, already at greater risk of ill effects from the virus, died in large numbers in the early outbreaks, which disproportionately struck rural nursing homes and other long-term care facilities.

4. Mask requirements sparked controversy. While many public health and hospital officials called for statewide requirements for mask wearing. Gov. Brian Kemp stood firm against that, saying masks should be encouraged but not mandated. That brought him into conflict with Atlanta Mayor Keisha Lance Bottoms, who required masks in public in the city. Kemp argued that that the mayor’s mask mandate violated his emergency order prohibiting localities from being more restrictive than the state. The standoff eventually eased when Kemp withdrew a lawsuit against city officials and the limits of the Atlanta rules were spelled out.
5. Pandemic plans and Affordable Care Act protections become campaign issues. Democrats accused President Trump and fellow Republicans of mishandling the pandemic. Republicans said the Democrats had taken inconsistent positions on the virus and had made errors in the states they controlled. Democrats also said that people with pre-existing conditions (covered by the ACA) were at risk from Republican policies, though GOP candidates said they still planned to protect such people. Ultimately, the electoral results across the nation were less sweeping than analysts predicted, suggesting that health care controversies are by no means settled. But now all eyes are on Georgia and its two Senate runoff races, to be decided Jan. 5, which will determine which party controls the chamber.
6. Gov. Kemp’s waiver plans got federal approval. Kemp’s plan to add low-income Georgians to the Medicaid rolls would set fairly stiff requirements for eligibility, such as employment or other activities. A second waiver would allow a reinsurance program, which has lowered insurance premiums in other states. It also would replace healthcare.gov with a state-run, private insurance pathway to coverage. Critics, especially Democrats, said the governor’s Medicaid plan would deliver much lower enrollment numbers than a standard Medicaid expansion, which Kemp and other Republicans have long opposed. And some consumer groups slammed the second waiver plan, saying healthcare.gov has worked too well to be replaced.

7. A nursing home exec’s funding plan left Georgia on the hook with the feds. Ronnie Rollins used a controversial loophole to secure $300 million in bonus payments for his nonprofit nursing home chain. A federal investigation called the payments “inappropriate,” and Georgia is caught in a multimillion-dollar dispute. Though Rollins is not accused of wrongdoing, the feds say the state must now come up with $76 million to resolve the matter. Rollins and state officials have pushed back, and the issue hasn’t yet been resolved.
8. Coal ash and water contamination put a Middle Georgia town in the spotlight. Testing of private drinking wells in Juliette near Plant Scherer, the nation’s largest coal-fired power plant, has found contaminants in the water. Georgia Power, which runs the plant, said it has identified no risk to public health or drinking water. The company is trying to convince regulators to allow it to leave more than half of its coal ash in unlined ponds at plant sites spread across the state. Meanwhile, 45 Central Georgia residents claimed in a lawsuit that the utility has unlawfully released, discharged and deposited coal ash into their community’s drinking water source. And an investigation by Georgia Health News and ProPublica found that the utility paid over $15 million for nearly 1,900 acres close to five of its 12 power plant sites.

9. Lead poisoning from soil and older homes continued to be a widespread danger. A GHN investigation identified ZIP Codes with high percentages of children showing elevated levels of lead in their blood. These included urban areas, such as Savannah and Augusta, and rural parts of the state. The EPA, meanwhile, widened its investigation of properties in the westside of Atlanta that had dangerous levels of lead, a powerful neurotoxin, in their soil.
10. A state contract to supply health care workers went to a politically connected firm. A unit of Alpharetta-based Jackson Healthcare stood to earn more than $300 million from a state contract to supply nurses and other medical workers to hospitals and nursing homes in Georgia during the pandemic. The fact that the company got a no-bid contract after years of donating to leading Republican politicians led critics to claim favoritism. But the Kemp administration and the company said the arrangement was above board and had worked out well.