Most Georgians know the irritating sensation of not being able to breathe through their noses during cold or pollen season. It may be caused by chronic sinusitis or sinus infection, and most cases of both types clear up on their own.
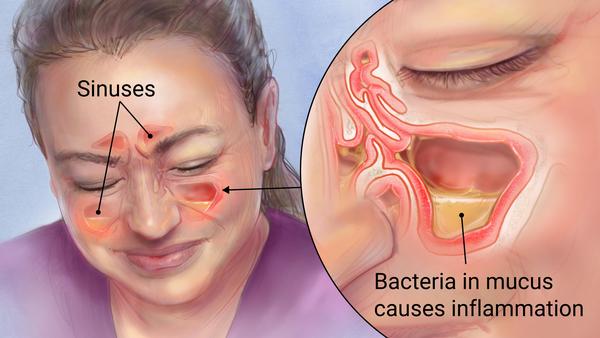
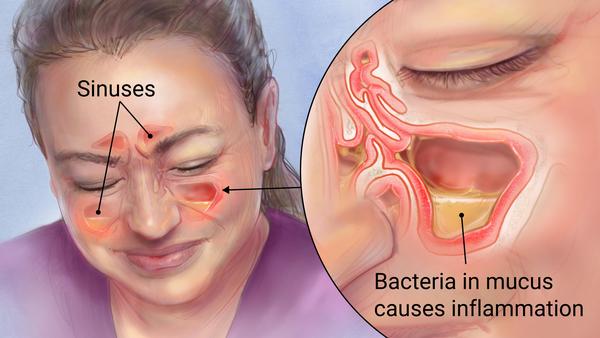
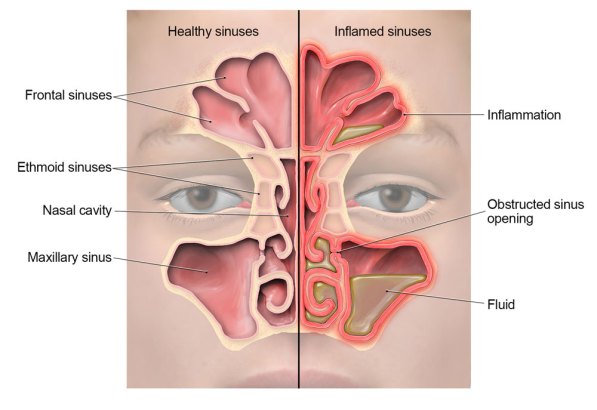
Sinus infections occur when cavities around the nose are inflamed, making breathing difficult. Though bacteria cause a small number of sinus infections, most are viral and should not be treated with antibiotics, according to the CDC.

Studies show that about three-quarters of patients who see doctors for sinus complaints leave with prescriptions for antibiotics. Unfortunately, these often don’t meet the prescribing guidelines that are meant to curb unnecessary use of the germ-fighting drugs.
This worries Dr. Mark Ebell, a Georgia physician, who is researching how sinus infection misdiagnosis — and subsequently antibiotic resistance — can be reduced.
Respiratory infections are the most common reason for antibiotic use in the United States, and of those, sinus infections are responsible for more unnecessary antibiotics than any other, according to Ebell, an epidemiology professor at the University of Georgia.
Ebell has developed a diagnostic tool to help physicians distinguish between viral and bacterial infections.
“Patients need to realize that most of these [sinus infections] are viral, and that antibiotics are only recommended if symptoms are severe or have lasted more than 10 days,” he says.
Signs that might indicate a bacterial sinus infection include pain on one side of the face, in the cheek and in the upper teeth, Ebell says. Someone who has a cold and begins to get better, but then starts feeling much worse, is another type of patient who may have a bacterial infection, he says.
Ebell has developed a clinical decision rule for diagnosing sinus infections. It incorporates patient symptoms and a simple blood test to more accurately detect bacterial infections.
The tool is the first of its kind, and he says it can help physicians and patients know when to reach for antibiotics, and most importantly, when not to do so.
Antibiotic resistance is a growing public health threat, and though it occurs naturally, it is being sped up by misuse of medication.
More than 2 million illnesses and 23,000 deaths have been caused by antibiotic resistance, according to CDC. Resistant bacteria make it harder to treat infections such as pneumonia, tuberculosis and gonorrhea.
The specter of antibiotic resistance
The World Health Organization warns that without urgent reduction of antibiotic misuse and overuse, we will enter a “post-antibiotic era” in which common infections and minor injuries can kill.
Ebell and Danish researcher Dr. Jens Hansen recorded symptoms and results from a blood test that reports C-reactive protein levels (CRP test) for 175 patients who showed signs of sinus infection, to determine patients’ likelihood of bacterial infection based on body inflammation.

The resulting “sinus score” gives physicians an easy-to-use threshold indicating if the patient is at low, moderate or high risk for bacterial infection. If all high-risk and half of moderate-risk patients were treated with antibiotics, about one-third of all sinus patients in the study would receive antibiotics, a dramatic contrast to current prescription practices of 75 percent.
Some bacterial infections require antibiotics. But because so many antibiotics have been pumped into our bodies and food since they gained mainstream use in the 20th century, bacteria have grown more and more resistant to drugs that once proved effective at killing the bugs.
“Primary care physicians are well aware that it’s a problem, and are concerned about it,” says Ebell. “However, patients have come to expect an antibiotic for all sinus infections, as well as many other respiratory infections, and doctors place value on having a satisfied patient.”
“But, while we have tools like the strep test to avoid antibiotics in patients with viral pharyngitis, and the influenza point-of-care test for patients with flu-like illness to avoid unnecessary use of [antibiotics], we have no such tools for patients with sinusitis or acute bronchitis,” he said.
Because sinus symptoms are a major patient concern, there is often stress and misinformation surrounding the diagnosis, says Dr. Eddie Richardson Jr., president of the Georgia Academy of Family Physicians.

“Patients want relief, and this is a customer service business,” says Richardson, who runs Lake Oconee Urgent and Specialty Care Center, when asked about Ebell’s research.
Richardson says respiratory issues increase to about 20 percent of his business during October. He says it can be difficult to explain to patients why their particular symptoms don’t warrant the use of antibiotics. “I try to get them symptomatic relief, like nasal sprays, before [possibly] putting them on antibiotics, and talk to them about how their environment might cause [allergy] exposure.”
Richardson says the time frame of a patient’s symptoms and the person’s history of allergies, plus what shows up in a physical exam, are important factors in whether he decides to prescribe antibiotics. A test that helps give objective data about sinus infection thresholds could help his patients understand why he makes his decision, he says.
More research is needed to test the sinus score in a clinical setting, but the CRP diagnostic tool is used in some European countries and in some U.S. labs.
There are still some practical obstacles to widespread use of the test. Most primary care settings do not have the “moderate complexity lab certification” to use the CRP test based on FDA regulations, and Ebell hopes studies like his will encourage the FDA to loosen these restrictions.
Ebell says the tool is a win-win for doctors, patients and society at large to help reduce antibiotic resistance.
“Doctors are generally asking these questions already, and the clinical decision rule helps them interpret the answers in a more meaningful, clinically useful way by combining the most informative signs and symptoms,” Ebell says. “While the CRP blood test would take about 5 minutes, if approved by the FDA, then [doctors] could bill for it and even make a small profit.”
The study, “Proposed Clinical Decision Rules to Diagnose Acute Rhinosinusitis Among Adults in Primary Care,” published in Annals of Family Medicine, is available online at http://www.annfammed.org/content/15/4/347.